Tags
Diagnosis, Dialysis, Doctor, eGFR, energy, Flood, health, Hemoglobin, Hospital, infusion, Iron, Kidney, kidney disease, kidney failure, Kidneys, Life, Medical, Nepgrologist, Oncologist, wellness
My nephrologist called me the other day to reschedule my appointment. Apparently, the hospital had a flood on the top floor, and their offices were flooded as well. Because when you’re already dealing with kidney issues, why not throw in some surprise indoor rain?
As a result, they had to temporarily move their offices to one of their satellite locations in a nearby city. The day before my appointment, they called again and asked if we could just do a teleconference instead. Same time, same doctor, no driving, and no pants required from the waist down—absolutely.
My lab work had already been done a couple of weeks earlier, and because I like to mentally prepare myself for either good news or emotional damage, I had my results emailed directly to me. Now, I’m not a doctor, and I don’t pretend to understand every number on those reports, but there are a few that I follow very closely.
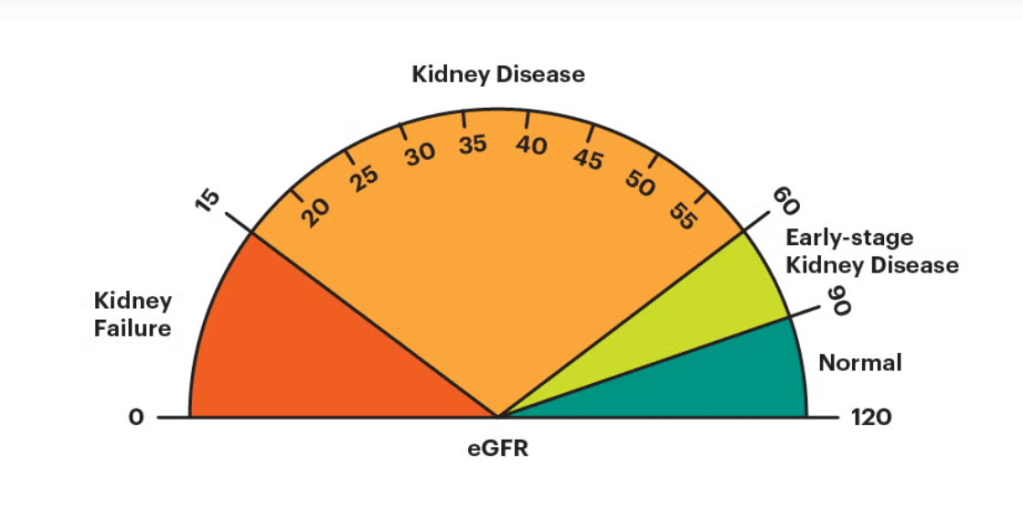
First up is eGFR, or estimated Glomerular Filtration Rate. This number tells you how well your kidneys are filtering your blood. A normal range is between 90 and 120—numbers I personally haven’t seen in a while and would probably frame if they ever showed up again.
- 60–89 is Stage 2 kidney disease
- 45–59 is Stage 3a
- 30–44 is Stage 3b
- 15–29 is Stage 4
- Below 15 means kidney failure, and dialysis becomes a very real conversation
Then there’s Creatinine, a waste product filtered by the kidneys. In simple terms, the higher the number, the worse things are working. Think of it as your kidneys’ performance review—lower is better.
The last big number I keep an eye on is hemoglobin, the protein responsible for carrying oxygen throughout your body. This one has a direct impact on how much energy I have, which explains why some days I feel like I could conquer the world, and other days I need a nap after tying my shoes. Normal range is 13.2-17.1
So here are the numbers I focus on:
- eGFR: 35
- Creatinine: 2.09
- Hemoglobin: 10.5
Now yes, an eGFR of 35 doesn’t exactly scream “picture of perfect health,” but context is everything. Last year, that number was 14. At that point, my doctor was already talking about my next visit being with a dialysis specialist. That’s not a meeting you look forward to.
So going from 14 to 35? I’ll call that a solid upgrade.
My creatinine also improved significantly—from 4.29 last year down to just over 2. Another small victory, but I’ll gladly stack those wins wherever I can get them.
Hemoglobin, however, continues to do whatever it wants. It fluctuates so much that I regularly need iron infusions. My oncologist thinks it’s related to my kidney function, while my nephrologist believes it’s tied to the chemo drug I’m on. At this point, I feel like the two of them should arm wrestle, and whoever wins gets to be right.
When the call wrapped up, my nephrologist said she was happy with where things are. She even used the word “stable.”
And if you’ve never dealt with chronic illness, “stable” might sound underwhelming. But when you live in this world, stable is a beautiful word.
Stable means no dialysis—for now.
Stable means nothing is getting worse.
Stable means today is better than last year.
So yeah, I’ll take stable.
No complaints.
And preferably without any more floods—indoor or otherwise.
Discover more from Grayfeathersblog
Subscribe to get the latest posts sent to your email.

My very first repeat Echocardiogram (as you said context is everything, a number does not mean as much unless you can compare it to another number) is in 4 weeks (for bi-leaflet mitral valve prolapse resulting in moderate—borderline severe— regurgitation), and I am hoping for a “stable” also. Omg, stable will be like winning an award!
Here’s to a “Stable” report for you also!!